Perioperative Anaphylaxis

Recognizing Anaphylaxis in the Perioperative Environment
Anaphylaxis in the perioperative environment is a rare occurrence, however it requires immediate recognition and treatment. Anaphylaxis is a life-threatening emergency in response to a trigger factor, usually with symptoms developing quickly after exposure to the triggers such as food, medications or insect venom. Within the perioperative environment, anaphylaxis is most commonly associated with the administration of medications. As most medications are administered intravenously, the onset of symptoms is often rapid and needs to be managed to prevent further clinical deterioration. Frequent triggers within the perioperative environment included antibiotics, neuromuscular blocking agents and chlorhexidine.
Grading Anaphylaxis Severity
Grading of anaphylaxis severity is as follows:
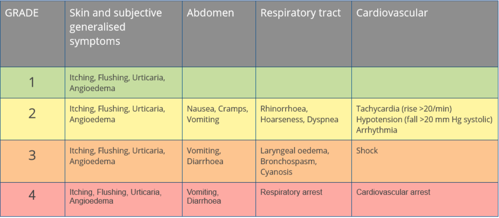
Adapted from Worm et al (2014) https://doi.org/10.3238/arztebl.2014.0367 modification of Ring and Messmer 1977
For patients who have Grade III (severe) anaphylaxis, the cutaneous signs are often absent as perfusion to the skin is inadequate to produce symptoms. Additionally, central nervous symptoms of lightheadedness, confusion and a sense of impending doom are associated with hypotension and poor perfusion to the brain. In the perioperative settings, conditions such as anaesthesia and draping may obscure early signs of anaphylaxis as the patient is unable to report symptoms, and drapes may obscure visualisation of skin changes.
Treatment of Anaphylaxis
Once anaphylaxis has been identified, immediate treatment is required to stop the allergic cascade from producing histamines, prostaglandins and cytokines, and manage the effects of these agents. Management will include immediate treatment, refractory management and post crisis management. The Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG) have worked together to produce Anaphylaxis cognitive aids for these stages of management in both adult and paediatric patients. Each of these cards should be printed and laminated for easy access during anaphylaxis, preferably located in/next to the anaphylaxis emergency box.
Treatment of anaphylaxis:
- Stop/remove trigger, including any infusions, synthetic colloids and chlorhexidine
- Send for help: get further assistance from colleagues, bring anaphylaxis emergency box, assign team leader and other roles
- Secure airway and support breathing: consider early intubation if not already intubated, stop anaesthetic inhalation gases and administer 100% oxygen
- Support circulation: elevate legs if hypotensive, ensure rapid fluid bolus administration (2 L crystalloid for adults, 20 mL/kg crystalloid for paediatrics), ensure large bore IV access and warm fluids if possible
- Administer adrenaline (epinephrine): IM or IV depending on the severity, consider infusion depending on response and age of patient, please see management cards for all dosing recommendations (links are in the reference section below)
- Cardiac arrest: if the patient becomes pulseless initiate Advanced Life Support guidelines as per ANZCOR paediatric or adult algorithm. In an adult cardiac arrest situation, ANZCA guidelines recommend IV adrenaline 1 mg every 1-2 minutes. In a paediatric cardiac arrest situation, ANZCOR guidelines recommend IV adrenaline 10 mcg/kg may be given every 1-4 minutes.
Learn More about Anaphylaxis and Perioperative Emergencies
If you would like to learn more about anaphylaxis and other perioperative emergencies, join us for our range of Anaesthesia and Recovery Room Nursing courses. Our 2021 courses include:
Article reviewed August 2023 by Susie Helmrich.
References:
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Perioperative Anaphylaxis Management Guidelines.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Perioperative Anaphylaxis Management Guidelines Background Paper.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Adult Immediate Management Card.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Paediatric Immediate Management Card.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Adult Refractory Management Card.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Paediatric Refractory Management Card.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Differential Diagnosis Card.
Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group (ANZAAG). 2016. Post Crisis Management Card.

Crystal Smith is a Senior Education Consultant for Critical Care Education Services (part of the Medcast Group). She has a clinical background in critical care, paediatrics and education.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreCarl has been in ICU for 2 weeks, over the last 24 hours his condition has deteriorated. What priority assessment needs to be done to get to the bottom of Carl’s deterioration and optimise his plan of care?
A 67-year-old male with a history of hyperlipidaemia and hypertension, presents with dizziness. He has a fast atrial rate and irregular heart rhythm. This article highlights causes, risk factors, complications, and management strategies, emphasising stroke prevention through anticoagulation and lifestyle modifications.
Understand the requirements of the updated RACGP recommendations for the Doctor’s Bag to stay compliant and prepared for your next clinical emergency
