The ABCDE of post resuscitation care
“There’s signs of life” announces one of your team members following the third rhythm check in the resuscitation of Nadia Grey. Nadia has had CPR for the past 10 minutes, and has received 2 shocks at 200 joules each for VT. The defib was disarmed following the COACHED safe defibrillation sequence, and an organised rhythm, increased EtCO2 and some respiratory effort had been seen.
What is your plan of care for Nadia now?
Immediately perform an ABCDE assessment now that Nadia has return of spontaneous circulation (ROSC).
To minimise the risk of Nadia rearresting and ensure the best possible outcome for her, it is important to follow an ABCDE assessment once she has return of spontaneous circulation (ROSC).
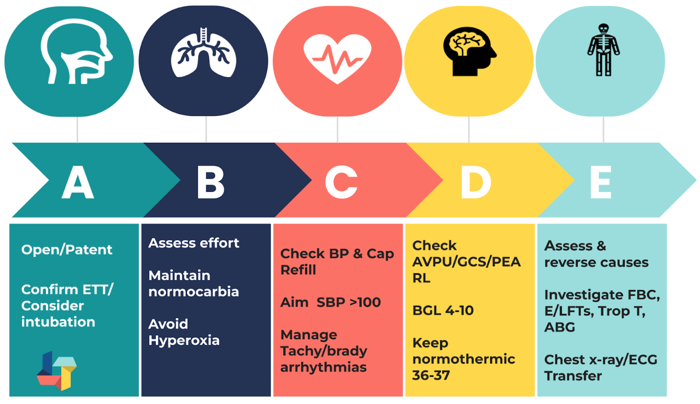
Airway
Check for airway patency. If not already performed during the resuscitation, consider intubation or SGA (if skilled clinician not available) in those patients who remain comatose following ROSC, or who have another clinical indication for sedation and mechanical ventilation. Confirm placement with waveform capnography and maintain EtCO2 35-45 mmHg.
Following brief episodes of cardiac arrest with an immediate return of normal cerebral function and breathing at ROSC, an advanced airway may not be necessary if the patient is able to maintain their own airway.
Breathing
Use the “RATES” mnemonic to ensure a complete assessment of breathing.
- Rate: Count the patient’s own respiratory rate and supplement patient breaths with a bag-valve-mask (BVM) if bradypnoeic.
- Auscultate: Listen to the patient’s chest for presence of abnormal breath sounds or absence of breath sounds.
- Trachea: Check whether the trachea is midline (if not, may indicate tension pneumothorax) or presence of tracheal tug (respiratory distress).
- Effort: Look for accessory muscle use indicating respiratory distress e.g. intercostal or subcostal recession, and (in paediatrics) nasal flaring, head bobbing and grunting.
- Saturations: Maintain the patient’s SpO2 between 94 - 98% with oxygen via a facemask.
Circulation
Check Nadia’s heart rate and rhythm, as well as her BP and central capillary refill. Consider vasopressor / inotropes and/or IV fluids if she is hypotensive (aim for SBP > 100 mmHg). If she has symptomatic bradycardia or tachycardia follow the appropriate management algorithms.
If an antiarrhythmic drug was used successfully during the resuscitation this should be continued.
If no antiarrhythmic drug was administered during resuscitation from a shockable rhythm, this should be considered at ROSC to prevent recurrent VF.
Disability
Perform a neurological assessment, including pupils, and monitor BGL to maintain normoglycaemia. Administer insulin for BGLs >10 mmol/l. Treat any seizure activity with sedation and/ or anti-epileptic drugs.
Exposure
Monitor temperature and prevent fever for at least 72 hours. Check for any signs of bleeding or infection including wounds and drains. Also check Nadia’s skin for any signs of rash or bites. Palpate her abdomen for signs of distension and firmness.
Further investigations:
- Reassess reversible causes and any lines or drains inserted during resuscitation
- Organise appropriate inter or intra-facility transfer
- Blood tests including FBC, electrolytes, CKMB, Troponin T and ABG/ VBG
- ECG. Consider Coronary angiography ± PCI if likely cardiac cause, and if not, CT brain and/or CTPA.
- CXR
- Echocardiography
Delay prognostication for at least 72 hours.
References
ANZCOR (2024). Guideline 11.7 – Post-resuscitation Therapy in Adult Advanced Life Support. Retrieved May 2024. guideline-11-7-post-resuscitation-therapy-in-adult-advanced-life-support-250.pdf (anzcor.org)
Nolan, J., Sandroni, C., Böttiger, B., Cariou, A., Cronberg, T., Friberg, H., Genbrugge, C., Haywood, K., Lilja, G., Moulaert, V., Nikolaou, N., Olasveengen, T. M., Skrifvars, M.B., Taccone, F., and Soar, J. (2021). European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post‑resuscitation care. Intensive Care Med, (47). 369–421 https://doi.org/10.1007/s00134-021-06368-4
Resuscitation Council UK (2023) Post- resuscitation care guidelines. Retrieved May 2024. Post-resuscitation care guidelines | Resuscitation Council UK
Related courses
Critical Bytes - Resuscitated, Now what? - In this webinar we will hear from experts who manage patients in the post-resuscitation care phase and explore the different approaches to stabilising patients for transport, whether that be to CT, ICU, to another hospital or interstate.

Jenny Browne, RN, Cert IV (TAE), CritCareCert, MN(AdvClinEd), has an extensive background in critical care nursing and education. Jenny has worked across a variety of Australian ICUs, including the John Hunter Hospital (Newcastle), Princess Margaret Hospital (Perth) and the Royal Adelaide Hospital. She has been an ALS and PALS instructor for over 12 years, including with the ACCCN, and is also a sessional academic at the University of Newcastle.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreFollow James, a 7-year-old boy scheduled for a tonsillectomy and adenoidectomy, as we explore how the 4 P’s of child preparation – Prepare, Play, Parent, Praise – can be used in day surgery to reduce procedural anxiety, support family-centred care, and improve the overall patient experience
Caregiver concern is a powerful predictor of clinical deterioration in children, often surpassing abnormal vital signs. A recent Lancet study confirms its association with ICU admission and ventilation. Integrating caregiver input into assessments, documentation, and escalation protocols can significantly improve early recognition and outcomes in paediatric emergency care.
Sepsis is a time-critical medical emergency. The National Sepsis Program urges GPs and primary care clinicians to enhance early recognition and management of sepsis to save lives. This update outlines key actions and available resources to support timely diagnosis and intervention across primary care settings.
