
Terminal care: management of pain and respiratory secretions - clinical fact sheet and MCQ
Overview
Terminal care is the care and support provided to a person and their family/carers in the final days or weeks of life, and focuses on comfort, symptom management, and quality of life.
The Prompts for End-of-Life (PELP) Planning tool supports proactive planning for the last 12 months of life. It provides a framework with suggested components of a terminal care management plan that considers symptom control, anticipatory prescribing, and other issues which complement this Fast Track.
A consensus-based list of the core medications used for managing terminal symptoms is found here.
Epidemiology
In Australia, more than 160,000 people die each year. Most deaths are expected and follow a period of chronic illness, during which end-of-life care becomes essential. General practitioners play a key role in delivering this care, especially in community settings.
General principles
Terminal care needs to be holistic, encompassing physical, psychological, social, and spiritual domains. It aims to:
- maintain comfort and dignity
- manage distressing symptoms
- respect patient preferences and goals
- support families and carers
Medications may be used during the terminal phase of care:
- in anticipation of common terminal symptoms
- for ongoing management of pre-existing symptoms
- to address emergent symptoms with additional medication dosages
Any medications prescribed during terminal care should be regularly reviewed to ensure adequate symptom control. All medications not directly contributing to patient comfort can be ceased.
Oral administration of medications often become difficult at the end of life due to swallowing issues, vomiting, or reduced consciousness. This is the time to transition to subcutaneous administration via intermittent injections or continuous infusion, which is considered to be the most reliable route in these patients.
To calculate dose equivalencies, use the equianalgesic opioid calculator in the palliMEDS app.
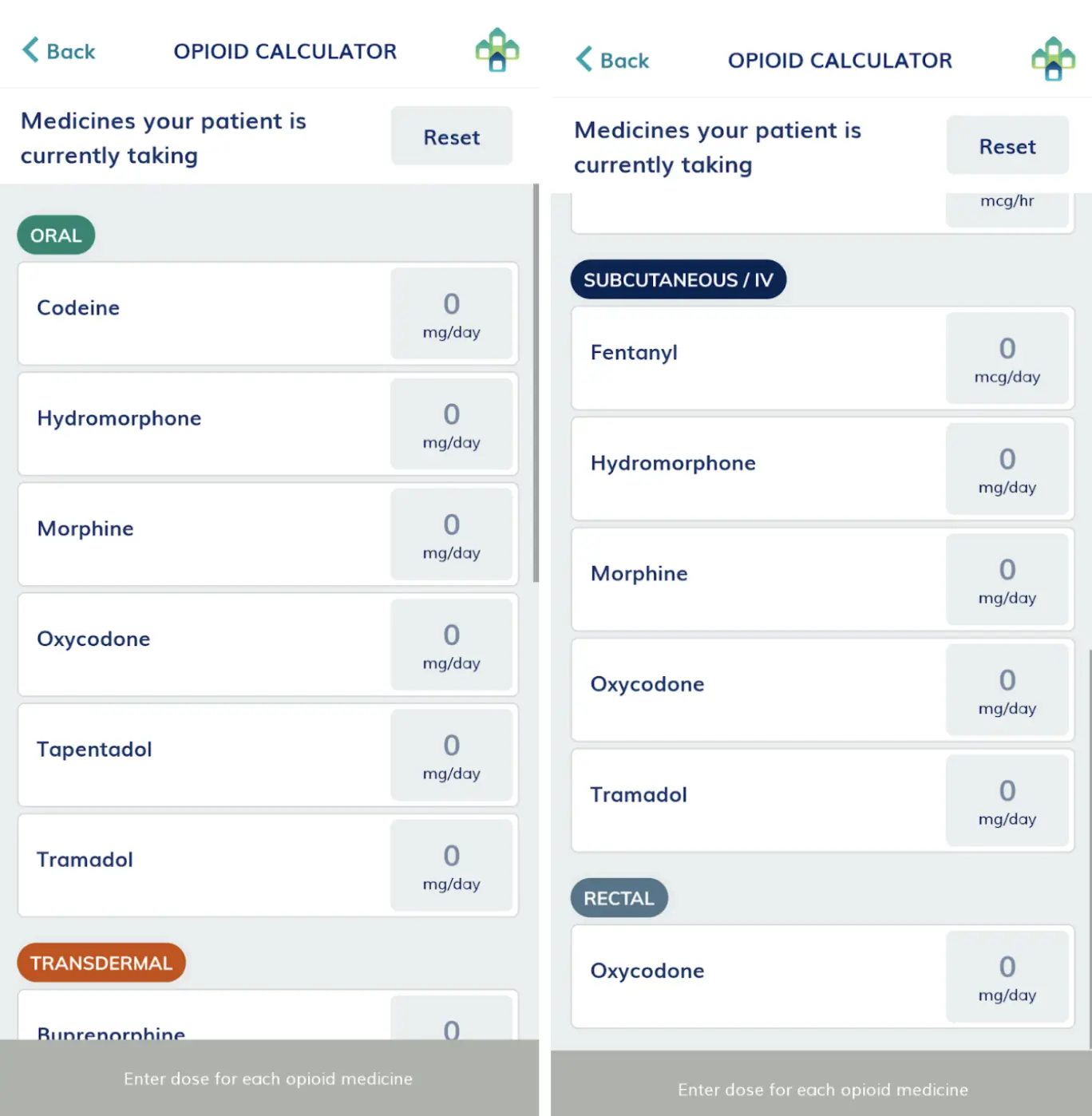
Image 1: the equianalgesic opioid calculator from the palliMEDS app
Sometimes, ethical dilemmas can arise when prescribing analgesia in terminal care. The doctrine of double effect provides legal protection applicable only for patients in the terminal stage of care. It states that appropriately prescribed analgesia or symptom relief may unintentionally hasten death, but is ethically and legally acceptable if the intention is to relieve suffering and not to cause death. A comprehensive introduction to end-of-life laws for clinicians can be found here, applicable to all Australian states and territories.
Morphine for pain management in terminal care
Pain at the end of life is often multifactorial. In terminal care, the goal is to maintain comfort and balance analgesia with preservation of alertness where desired.
Specific recommendations for the use of morphine injections (sulfate or hydrochloride) for pain and dyspnoea can be found in the palliMEDS app.
General considerations:
- many opioids used in palliative care are prescribed off label, such as for the relief of dyspnoea
- this practice is supported by clinical evidence and is considered appropriate when consistent with best practice and patient-centred care
- however, there may be financial implications as off-label use is not subsidised through the Pharmaceutical Benefits Scheme
- consider starting with a morphine dose towards the lower end of the recommended range for older and frail patients, due to greater opioid sensitivity
- monitor for sedation, confusion, nausea, constipation, and respiratory depression
- engage with patients and families about goals of care and expected effects
Anticipatory prescribing
Patients in the last weeks or days of life should have subcutaneous PRN medications prescribed pre-emptively to avoid delays in treating the common symptoms that occur, even if the patient is already on regular opiates. It is particularly important to consider anticipatory prescribing for predictable episodes of pain, such as those related to dressing changes or movement.
For pain, in opioid-naive patients, this is usually morphine 2.5-5 mg subcutaneously every hour as required. If the patient is already on opiates, it is usual to start with 1/10th of the regular dose. Adjust dose and frequency as required. Reconsider therapy if more than three doses are required over 24 hours.
If the pain is ongoing, consider increasing the dose and using a continuous subcutaneous infusion delivered over 24 hours.
Breakthrough pain
For all patients, an additional hourly dose can be administered as required for breakthrough pain
Non-pharmacological pain management can supplement morphine in terminal care and includes:
- repositioning for pressure relief
- heat or cold packs
- relaxation techniques or guided imagery
- involvement of allied health professionals for massage or supportive therapy
Morphine for dyspnoea in terminal care
Morphine reduces the sensation of breathlessness by altering central perception and reducing ventilatory drive. Low doses, titrated to effect, work even in the absence of pain. Monitor for sedation and ensure the patient’s positioning optimises ventilation.
- Regular prescribing for opioid-naive patients with dyspnoea:
- 1-2.5 mg subcutaneously every 4 hours, and 1-2.5 mg hourly, for breakthrough dyspnoea as required OR
- 5-10 mg over 24 hours by continuous subcutaneous infusion, and 1-2.5 mg hourly, for breakthrough dyspnoea as required
- Regular prescribing for patients already on opioids for pain management with intermittent dyspnoea:
-
- Use the pain breakthrough opioid dose to manage these dyspnoea episodes
Adjust dose and frequency as required. Reconsider therapy if three doses are required over three hours, or > 6 doses required in 24 hours, or if non-response.
- Ongoing dyspnoea:
- Consider increasing regular opioid dose by 25-50%
- Consider increasing regular opioid dose by 25-50%
Indications for referral
Refer to palliative care specialists when:
- pain is refractory despite opioid titration
- complex multimodal analgesia is required
- there is significant opioid toxicity or intolerance
Hyoscine butylbromide for respiratory tract secretions in terminal care
Commonly referred to as the ‘death rattle’, noisy breathing results from the accumulation of oropharyngeal and bronchial secretions due to reduced consciousness and loss of swallowing reflex. It is usually more distressing to families than to the patient.
Recommendations on the use of hyoscine butylbromide injections for respiratory tract secretions can be found in the palliMEDS app.
- Anticipatory prescribing: or prescribing for intermittent symptoms, if an anticholinergic medicine is clinically appropriate:
- 20 mg subcutaneously every 2 hours
Consider ceasing therapy if no improvement within 24 hours, or if causing adverse effects such as a dry mouth.
- Regular prescribing if patients have previously responded well to anticipatory prescribing:
- 20 mg subcutaneously every 4 hours OR
- 60-80 mg over 24 hours by continuous subcutaneous infusion
- Monitor response and adjust dose as required for regular prescribing
- Usual maximum dose within 24 hours is 120 mg
- Best results occur when started early, before secretions become established
- Less effective for thick tenacious secretions; these may require other strategies such as hydration review or suction (limited role)
- Monitor for anticholinergic side effects: dry mouth, urinary retention, blurred vision, delirium
Non-pharmacological management of respiratory secretions in terminal care:
- repositioning the patient laterally can help secretions drain
- reducing or stopping non-essential IV/enteral fluids can limit further accumulation
- provide reassurance to families about the benign nature of the symptom to the patient
References
- Therapeutic Guidelines. Principles of pharmacological management of pain in palliative care. 2024. Available at: https://app.tg.org.au/viewTopic?etgAccess=true&guidelinePage=Palliative%20Care&topicfile=palliative-care-overview&guidelinename=auto§ionId=c_PCG_Pharmacological-management-of-pain-in-palliative-care_topic_20#c_PCG_Pharmacological-management-of-pain-in-palliative-care_topic_20. (last accessed August 2025).
- CareSearch. Respiratory secretions. 2024. Available at: https://www.caresearch.com.au/Evidence/Clinical-Evidence-Summaries/Respiratory-Secretions. (last accessed August 2025).
- Best Practice Advocacy Centre New Zealand. Managing excessive respiratory secretions in the last days of life. 2023. Available at: https://bpac.org.nz/2023/last-days-of-life/respiratory.aspx. (last accessed August 2025).
- Sinha A, Vashisht R. End-of-Life Evaluation and Management of Pain. [Updated 2023 Feb 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568753/. (last accessed August 2025).
- CareSearch. Pain. 2024. Available at: https://www.caresearch.com.au/Evidence/Clinical-Evidence-Summaries/Pain. (last accessed August 2025).
- Therapeutic Guidelines. Assessing pain in palliative care. 2024. Available at: https://app.tg.org.au/viewTopic?etgAccess=true&guidelinePage=Palliative%20Care&topicfile=palliative-care-overview&guidelinename=auto§ionId=c_PCG_Assessing-pain-in-palliative-care_topic_2#c_PCG_Assessing-pain-in-palliative-care_topic_2. (last accessed August 2025).
- Therapeutic Guidelines. Principles of managing pain in palliative care. 2024. Available at: https://app.tg.org.au/viewTopic?etgAccess=true&guidelinePage=Palliative%20Care&topicfile=palliative-care-overview&guidelinename=auto§ionId=c_PCG_Principles-of-managing-pain-in-palliative-care_topic_17#c_PCG_Principles-of-managing-pain-in-palliative-care_topic_17. (last accessed August 2025).
- End of life Directions for Aged Care. Factsheet: Legal protection for administering pain and symptom relief. 2025. Available at: https://www.eldac.com.au/Our-Toolkits/End-of-Life-Law/Legal-Protection-for-Administering-Pain-and-Symptom-Relief/Factsheet#:~:text=What%20is%20double%20effect%3F,pain%20and%20not%20hasten%20death. (last accessed August 2025).
- CareSearch. Palliative medicines. 2024. Available at: https://www.caresearch.com.au/Health-Professionals/Nurses/Clinical-Care/Medicines-Management/Palliative-Medicines. (last accessed August 2025).
- CareSearch. End-of-life symptoms. 2025. Available at: https://www.caresearch.com.au/Health-Professionals/General-Practitioner/The-Dying-Patient/End-of-Life-Symptoms#:~:text=Excessive%20secretions-,Anticipatory%20prescribing%3A,(PBS%20%2D%20palliative%20care%20listing). (last accessed August 2025).
Expand your expertise
End-of-life planning Mini Audit
End-of-life care is a deeply important aspect of general practice. It requires clinical skill, compassion, and clear communication. This practical, reflective learning activity is designed to support general practitioners in delivering best practice care to patients approaching the end of life.
Claim your CPD
After reading the clinical summary above and reviewing the references, complete the quiz to gain 30 minutes of EA CPD and 30 minutes of RP CPD.
You can either self-report CPD to your CPD home, or Medcast will track your learning via your personal CPD Tracker and you can download and report these points once a year. See our CPD Tracker FAQ.
Quiz
Please log in or sign up for a free Medcast account to access the case study questions and achieve the CPD credits.
The Medcast medical education team is a group of highly experienced, practicing GPs, health professionals and medical writers.
MyMedicare is now part of routine general practice, with practical implications for billing, continuity of care, and practice systems. This FastTrack clarifies important points regarding eligibility, impacts on the GPCCMP billing, and how to avoid rejected claims. 30mins each RP and EA available.
Many GPs may not see veterans frequently. This FastTrack provides a summary of key steps that can make veteran care efficient, rewarding and well-integrated into routine practice, including links to additional resources. 30mins each of RP and EA are available.
From the 1st Nov 2025, updates to the MBS affect all GPs providing services related to long-acting reversible contraceptives. This FastTrack will get you up to date on which items attracted an increased rebate, the new item number, and how to avoid common compliance pitfalls. 30mins each of RP and EA CPD available with the quiz.
