From service to community: essential steps to integrate veteran care into your practice
![]()
As the first point of contact with primary care after completing service, general practitioners are well placed to support veterans as they transition from military service to civilian life. Early identification of veteran status, structured assessment, and coordinated care can significantly improve health outcomes and support a successful transition.
Many GPs may not see veterans frequently. This FastTrack provides a summary of key steps that can make veteran care efficient, rewarding and well-integrated into routine practice.
![]()
Step 1: identifying veterans and their families in your practice
Identifying veterans is the first step in delivering coordinated care. This can be easily embedded into routine practice systems, such as new patient registration forms or health history updates.
Simple screening questions include:
- have you ever served in the Australian Defence Force (ADF)?
- do you have a Veteran Card?
Based on the DVA card a veteran may have, different eligibility criteria may apply. If your patient has served but doesn’t have a Veteran Card, ask them to contact DVA to check if they’re eligible for funded health care and support.
- A Veteran Gold Card: covers funding of clinically required medical treatment for all medical conditions
- A Veteran White Card: covers funding of treatment for DVA-accepted service-related injuries or conditions and provides Non-Liability Health Care (NLHC) for mental health conditions (and cancer, if eligible)
Those with a Veteran White Card can provide their GP with a printed or emailed list of accepted conditions obtained from their MyService account. It is also appropriate to ask about dependent family members, who may be eligible for additional DVA-funded support.
Step 2: completing the Veterans’ Health Check (VHC)
Veterans may be eligible for two types of health assessments, depending on their service. Some veterans may access both.
One-off Veterans’ Health Check
All veterans who have separated from the ADF after at least one day of continuous full-time service (including reservists) are eligible for a once-off health assessment using standard MBS time-based items (701–707).
- A DVA Veteran Card or DVA client number is required for DVA to fund the appointment
- The assessment must include components as outlined on the Veterans’ Health Check webpage
Annual Veterans’ Health Check
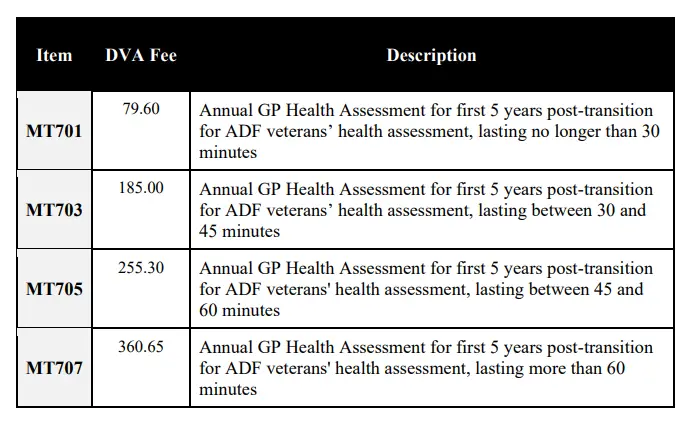
Table 1: DVA-related item numbers (source: https://www.dva.gov.au/sites/default/files/2026-01/dva-medical-services-schedules-1-jan-2026.pdf)
Eligible veterans may receive an annual VHC for up to five years post-discharge, provided they:
- separated from the ADF after at least one day of continuous full-time service (including reservists)
- transitioned out of the ADF on or after 1 July 2019
DVA-specific item numbers (MT701–MT707) must be used, and the consultation must be bulk billed to DVA; no gap payment can be charged.
- A DVA Veteran Card or DVA client number is required for DVA to fund the Annual Veterans’ Health Check appointment
- The VHC assessment must include components as outlined on the Veterans’ Health Check webpage
Key considerations for VHCs
- Allocate 45-60 minutes for the initial assessment
- Use a structured framework (eg, the Medcast VETERANS Lens) to guide whole-person care across physical, psychological, social, and occupational domains
- Screen for transition-related issues, including identity changes and adjustment to civilian life
- Discuss and document access to veteran service organisations (VSOs), DVA services, and veteran/family support hubs
Step 3: planning ongoing care
Many veterans require ongoing management for chronic conditions that are more prevalent in this population, including musculoskeletal conditions, hearing loss, tinnitus, cardiovascular risk, and mental health disorders. The following process can be used to support their ongoing care.
GP chronic condition management plan (GPCCMP)
A GPCCMP can formalise long-term goals, treatment strategies, and review schedules for veterans with chronic conditions. Planned reviews enable proactive care and timely adjustments.
Mental health care plans (MHCPs)
Under DVA NLHC, current and former ADF members who have completed at least one day of continuous full-time service can access funded treatment for any mental health condition without having to show a relation to service.
An MHCP can be used to provide coordinated care between the GP, psychologist, and psychiatrist. Psychiatric referral may be required for a formal diagnosis if there is a relationship to service and it is required for the DVA claims process (eg, PTSD).
If a psychiatrist is required, using the mental health care plan item numbers supports psychiatrists in billing item numbers.
Coordinated Veterans’ Care (CVC) Program
The CVC Program supports eligible Veteran Card holders with chronic conditions and complex care needs, including:
- Gold Card holders with one or more chronic health conditions
- White Card holders with a DVA-accepted chronic mental health condition
The full program eligibility criteria can be found in the Notes for CVC Program Providers.
The program involves enrolment, assessment of the patient, shared care planning with a care coordinator (eg, practice nurse), and regular reviews. The CVC Program aims to improve participant health and wellbeing, and reduce hospitalisations.
More information on the CVC Program can be found here.
Step 4: referrals for additional veteran specific supports
Consider referrals that address additional aspects of the veteran’s health:
- Treatment cycles: DVA-funded allied health treatment is provided in cycles (up to 12 sessions or 12 months) with a valid GP referral
- Rehabilitation Appliances Program (RAP): provides aids, equipment, and modifications to help eligible Veteran Card holders to live safely and independently
- Open Arms – Veterans & Families Counselling: free, confidential counselling for veterans and families
- Ex-service organisations (ESO): peer support and transition services (eg, Invictus Australia) can address identity, social connection, and wellbeing
- Client Support Program (CSP): supports veterans with complex or multiple needs to access DVA entitlements and critical support services
For other resources to integrate veteran care into your practice:
- Implementing the Coordinated Veterans’ Care Program in general practice webinar
- Medcast VETERANS Lens
References
- Royal Australian College of General Practitioners. What DVA‑funded services are available in general practice? 2022.. Available from: https://www1.racgp.org.au/newsgp/professional/what-dva-funded-services-are-available-in-general. (last accessed Nov 2025).
- Forbes D, Henderson C, Forbes S, Parslow R, Phelps A, O’Donnell M. Veteran and military mental health: the Australian experience. Curr Opin Psychiatry. 2014;27: 439‑44. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6735139
- Australian Institute of Health and Welfare. Veteran social connectedness: Introduction. Canberra: AIHW; 2023.. Available from: https://www.aihw.gov.au/reports/veterans/veteran-social-connectedness/contents/introduction. (last accessed Nov 2025).
- Flack M, Kite L. The “Transition” to civilian life from the perspective of former serving Australian Defence Force members. J Veterans Stud. 2023;9(1):129‑42. doi:10.21061/jvs.v9i1.407.
Claim your CPD
After reading the clinical summary above and reviewing the references, complete the quiz to gain 30 minutes of EA CPD and 30 minutes of RP CPD.
You can either self-report CPD to your CPD home, or Medcast will track your learning via your personal CPD Tracker and you can download and report these points once a year. See our CPD Tracker FAQ.
Quiz
Please log in or sign up for a free Medcast account to access the case study questions and achieve the CPD credits.
The Medcast medical education team is a group of highly experienced, practicing GPs, health professionals and medical writers.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreLifestyle medicine prescribing requires a specific approach for veteran patients that incorporates service-informed prescribing principles. This blog discusses the importance of lifestyle prescribing in veteran care while providing practical tips for GPs when formulating an effective management strategy for those who have served.
MyMedicare is now part of routine general practice, with practical implications for billing, continuity of care, and practice systems. This FastTrack clarifies important points regarding eligibility, impacts on the GPCCMP billing, and how to avoid rejected claims. 30mins each RP and EA available.
From the 1st Nov 2025, updates to the MBS affect all GPs providing services related to long-acting reversible contraceptives. This FastTrack will get you up to date on which items attracted an increased rebate, the new item number, and how to avoid common compliance pitfalls. 30mins each of RP and EA CPD available with the quiz.

