Post-operative fall - using an ABCDE assessment to identify risks
Marjory is a 68 year old in-patient who is 2 days post hip replacement. She is on rivaroxaban (xarelto) for VTE prophylaxis. You find her sitting on the floor of the bathroom, alert but in pain. She says she felt dizzy and then collapsed after she got up from the toilet
What is your initial action going to be?
ANSWER: Call for help and perform an ABCDE assessment (primary survey)
Prioritisation during clinical emergencies
There are several things to prioritise in this type of scenario, including determining the cause of the fall, and assessing for any ongoing concerns, injuries and complications?
Both the ABCDE and DRSABC can be helpful to guide decision making for the first moments of response. As you enter the scene, scan the environment for any dangers including body fluids, obstacles and access. Call for additional help including appropriate equipment to extricate Marjory from the bathroom.
Any patient who has had a fall needs to be assessed for head and neck injuries. Maintaining C-spine immobilisation with manual in-line stabilisation until injuries can be assessed and cleared helps to reduce the risk of further injury. Further assessment to determine the risk of cerebral bleed should include a review of medications such as antiplatelet, and antithrombolitic. We know that Marjory is on a DOAC - and this may increase her risk of bleeding.
After using the hover-jack and hover-mat to get Marjory from the bathroom floor to her bed safely. A primary and secondary survey using the ABCDE assessment tool is conducted to determine the cause of the fall, if there are any further injuries and to prioritise her care.
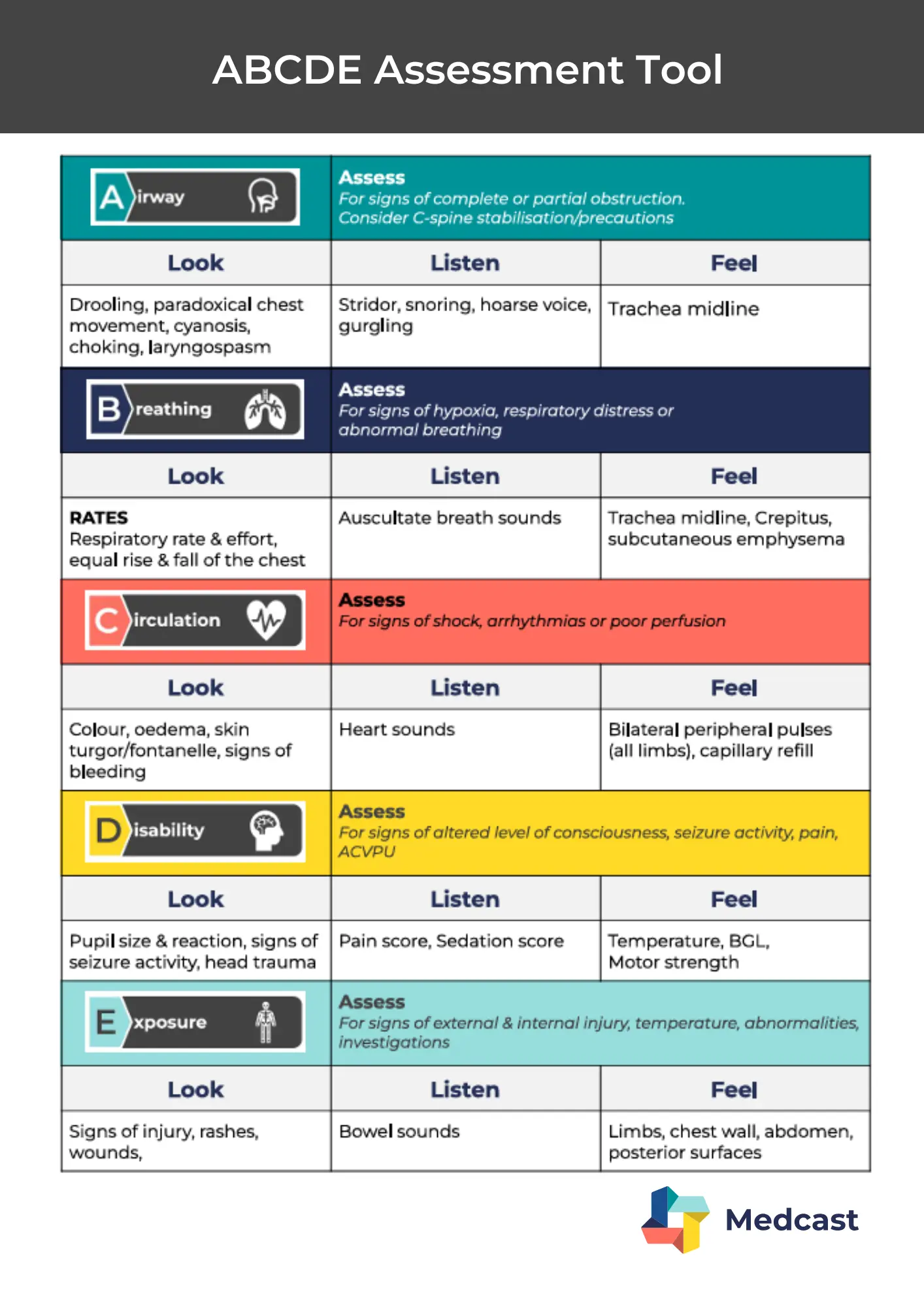
A - Airway
Look: no facial trauma or swelling. No drooling or cyanosis
Listen: Marjory is speaking clearly indicating a patient airway
Feel: trachea is midline
Interpretation: Airway is currently intact. No immediate intervention required. - Move on to assess B
B - Breathing
Look: respiratory rate 22, equal chest rise, no signs of respiratory distress
Listen: clear breath sounds bilaterally
Feel: chest expansion is symmetrical. No subcutaneous emphysema
Interpretation: No compromise in breathing. Continue to monitor, especially given the anticoagulant therapy which increases the risk of bleeding complications such as pulmonary contusion in blunt trauma. Move on to assess C
C - Circulation
Look: pale, no visible external bleeding. No bruising noted yet (ongoing assessment)
Listen: heart sounds present and regular - S1 S2
Feel: peripheral pulses equal, irregular, capillary refill 3 seconds, BP 105/65, HR 108
Interpretation: Red Flag - Marjory is on xarelto so occult bleeding (e.g. retroperitoneal or into the surgical site) must be considered. She is pale, tachycardic and hypotensive. Check Hb, consider fluid bolus monitor for delayed haematoma or signs of internal bleeding. Cardiac monitoring for irregular pulse.
D - Disability
Look: pupils equal and reactive to light
Listen: Marjory is oriented to person, place and time. No slurred speech or confusion
Feel: no motor deficits, reports pain 6/10 at surgical site, no limb weakness
Interpretation: Concern - Neurological status is normal, but Marjory has increased pain at surgical site, combined with her circulation status, this could be an indication of bleeding. Ongoing assessment for possible head injury is also important due to her fall and anticoagulation status
E - Exposure
Look: visual inspection reveals no head wound or lacerations. bruising over the hip noted
Feel: tenderness around the surgical site with mild swelling
Measure: Temp 35.9oC
Interpretation: Possible surgical site bleed or infection, organise imaging (x-ray of hip and CT head due to fall + anticoagulant therapy), bloods including full blood count and coagulation profile, 12 lead ECG due to irregular pulse
Communicating findings of ABCDE assessment
The ABCDE assessment tool provides a clear, structured approach that supports early recognition of deterioration. In high-risk situations like Marjory’s - recent THR, anticoagulation, and a fall - a systematic approach enables rapid escalation of care. Communication of the identified concerns and flags for Marjory should be via a clinical handover tool like ISBAR. From the assessment conducted, the clinical concerns that may have led to the fall or now be as a result of the fall include:
-
post-operative bleeding at surgical site
-
post-operative infection and sepsis
-
head injury/bleed
-
syncope from arrhythmia
Learn more and apply this approach to patient case studies in the following courses:
Lunch & Learn - Met call mayhem
Lunch & Learn - Anticoagulant management in surgical patients

Susan is the Head of Nursing Education for the Medcast Group.
DipAppScNsg, BN, CritCareCert, CoronaryCareCert, TraumaNsgCareCert, CertIV(TAE), MN(Ed), and GradCert(Ldrshp & Mgt).
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreFollow James, a 7-year-old boy scheduled for a tonsillectomy and adenoidectomy, as we explore how the 4 P’s of child preparation – Prepare, Play, Parent, Praise – can be used in day surgery to reduce procedural anxiety, support family-centred care, and improve the overall patient experience
Caregiver concern is a powerful predictor of clinical deterioration in children, often surpassing abnormal vital signs. A recent Lancet study confirms its association with ICU admission and ventilation. Integrating caregiver input into assessments, documentation, and escalation protocols can significantly improve early recognition and outcomes in paediatric emergency care.
Sepsis is a time-critical medical emergency. The National Sepsis Program urges GPs and primary care clinicians to enhance early recognition and management of sepsis to save lives. This update outlines key actions and available resources to support timely diagnosis and intervention across primary care settings.
