Paediatric Croup: Navigating Challenging Airway Scenarios
Understanding Childhood Croup: Identifying Symptoms
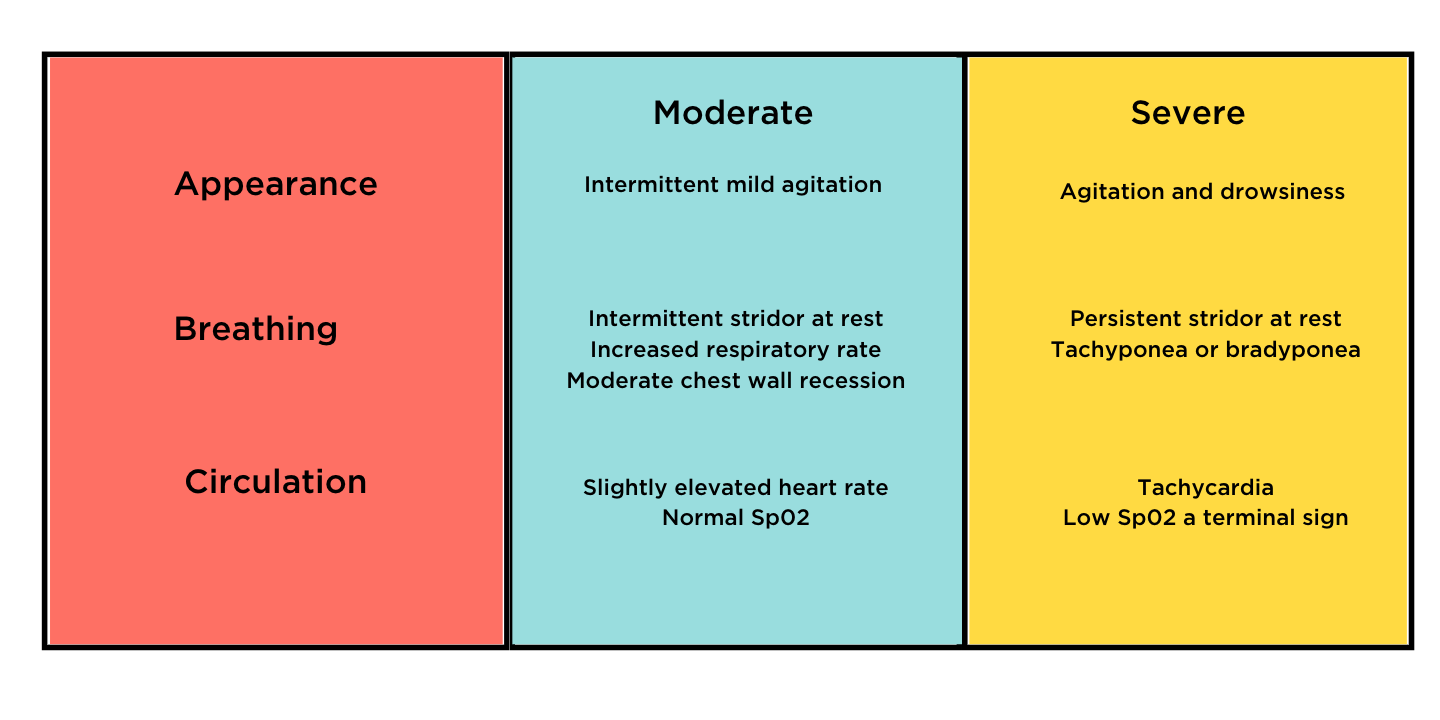
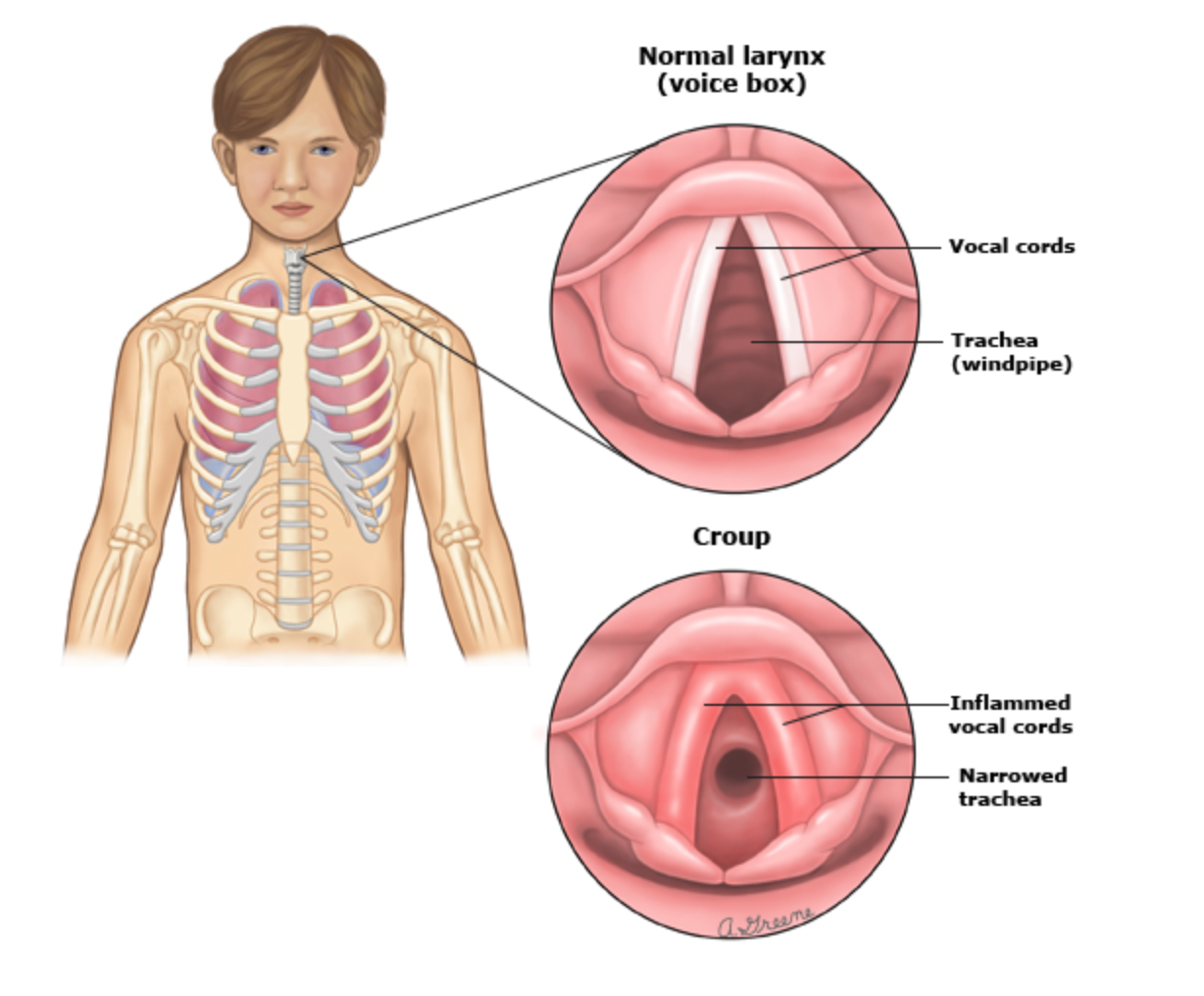
Croup is characterised by inflammation of the upper airways, leading to a distinctive barking cough, stridor, and respiratory distress.
On exam common signs and symptoms of croup include:
-
Barking cough
-
Inspiratory stridor
-
Hoarse voice
-
Associated widespread wheeze
-
Increased work of breathing
-
Fever, but no signs of toxicity
Although croup is common in children under 6 years and is often short lived and not life threatening. If the airway swelling progresses it can lead very quickly to a critical airway requiring intubation. Any distress in the child can quickly exacerbate the narrowed airway to complete obstruction so minimal handling is always recommended.
How do we determine if croup is progressing from a mild case to a life threatening airway emergency?
Croup can be classified into 3 categories of mild, moderate or severe. A common misconception with croup is that the louder the stridor the worse the airway is, but the opposite is true, with a quiet stridor more indicative of imminent airway closure. So knowing the assessment criteria is important to guide clinicians on how to best escalate care.
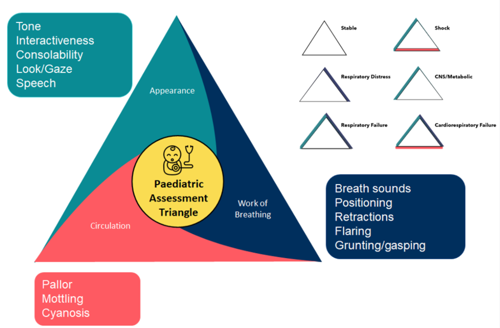
Assessing Croup Severity: The Paediatric Assessment Triangle (PAT)
The Paediatric Assessment Triangle (PAT) is a reliable and validated assessment tool that aids clinicians to determine the severity of a child's illness very quickly.
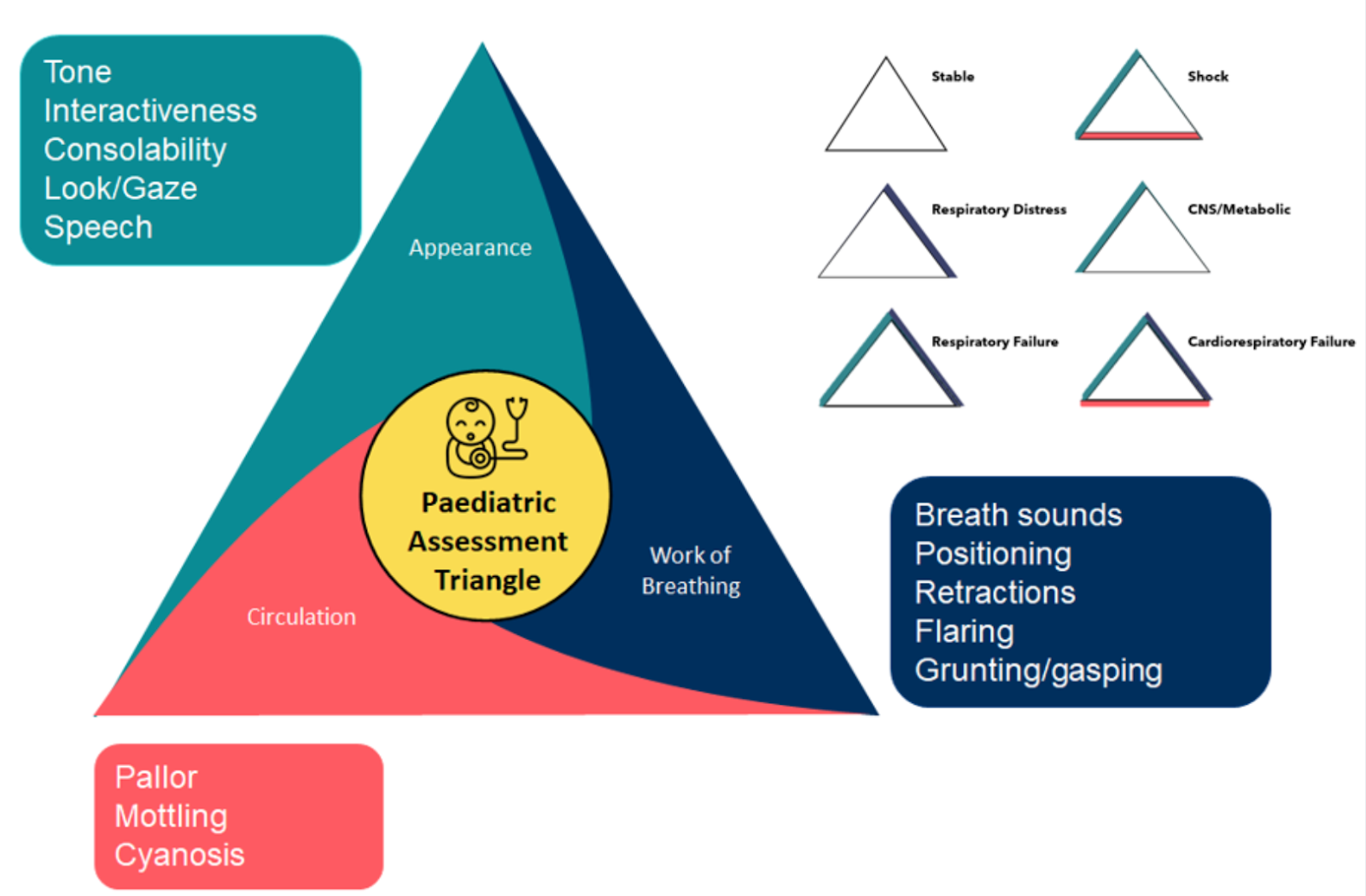
Applying the PAT to croup specific symptoms a moderate or severe case would appear with the following;
Treatment Protocols for Croup Cases
A moderate case would be treated with Dexamethasone 0.15 mg/kg orally or Prednisolone 1mg/kg orally.
As a case progresses into the severe phase, treatment includes nebulised Adrenaline 5mL of 1 mg in 1mL, and Dexamethasone 0.6mg/kg IV/IM/PO. If the child responds to the Adrenaline nebulisers they can be repeated, but escalation to specialist paediatric care is imperative as intubation of these airways is considered a difficult airway.
Children with moderate to severe upper airway obstruction are at high risk of deterioration and complete obstruction if they are upset, sedated or repositioned, so minimal handling of the child is warranted.
Challenges in Pediatric Intubation
Due to concerns for triggering complete airway obstruction, intubation usually involves keeping the child calm on the parents lap and using a sevoflurane gas induction followed by an IV insertion once the child has become sedated.
A tube size 0.5-1 mm smaller than the normal size for age may be required due to the swelling of the airways.
Further Learning and Related Courses
- Critical Bytes - Can’t Intubate, Can’t Oxygenate CICO
- PACED: Paediatric Assessment of Clinical Emergencies & Deterioration
- Paediatric Advanced Life Support (PALS)
- Assessing the unwell child with the Paediatric Assessment Triangle
- Paediatric Airway Emergencies
References
https://www.rch.org.au/clinicalguide/guideline_index/acute_upper_airway_obstruction/
https://www.rch.org.au/clinicalguide/guideline_index/croup_laryngotracheobronchitis/
https://www.uptodate.com/contents/croup-in-infants-and-children-beyond-the-basics/print

Grace Larson, RN, BN, CertIV(TAE), GradDipClinNurs(PaedCritCare), MAdNursPrac(PaedCritCare), has extensive experience in paediatric nursing, with 13 years in Paediatric Intensive Care Units (PICU). She’s published journal articles in the specialty area of pain and sedation in PICU, and has presented at national and international conferences on the area of pain and sedation in paediatrics. Grace has previously worked with the ACCCN delivering Paediatric Advanced Life Support in Victoria, bringing a wealth of experience into her clinical teaching on paediatric resuscitation. She has also consulted with NSW Health on quality and safety delivering within PICU, and has been contracted with the ANMF to develop nursing programs for nurses who require additional education as part of their practice requirements.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreIsaac is a 2 year old child who has presented to the GP for the fourth time this month. His previous presentations have been for a sore throat and fever and more recently food refusal and complaints of a sore stomach. His mother is very concerned, and rightly so, let's find out what’s happening with Isaac.
You have just received Stacey (6 years) to the paed’s unit following her tonsil and adenoid removal today.
Your next patient is Frankie, a 5 year old girl, who is brought in by her mother Nora. Frankie has been unwell for the past 48 hours with fever, sore throat and headache. The previous day Nora noticed a rash over Frankie’s neck and chest which has since spread over the rest of her body.