Maxine presents in respiratory distress
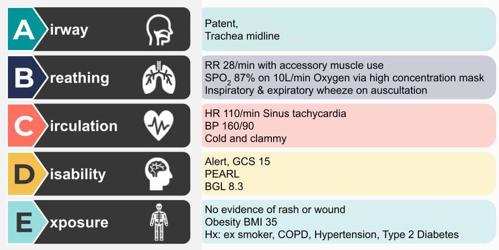
Maxine is a 63 year Kanamaluka woman who has presented to the emergency department with her daughter. She is complaining of increasing shortness of breath and difficulty breathing, and has been unwell for the last 3 days. Her daughter says Maxine has been coughing continuously and producing green phlegm.
Question
Which treatment modality would you recommend for managing Maxine’s acute respiratory failure?
-
Non-rebreather mask at 15 L/min
-
Non-Invasive Ventilation (NIV)
-
Intubation and mechanical ventilation
-
Chest physiotherapy and bronchodilators
NIV is a suitable treatment choice for Maxine’s acute respiratory failure due to its effectiveness in improving oxygenation, reducing work of breathing, and avoiding invasive measures. It is a well-established approach for managing COPD exacerbations and other causes of acute respiratory distress.
Acute Exacerbation of Chronic Obstructive Pulmonary Disease (COPD): Maxine's clinical presentation, including increased work of breathing, accessory muscle use, and wheezing, suggests an acute exacerbation of COPD. NIV is widely recognized as an effective treatment for COPD exacerbations, as it helps relieve respiratory distress and improves gas exchange without the need for invasive procedures.
Hypoxemic Respiratory Failure: Maxine's initial oxygen saturation (SpO2) of 87% on room air indicates significant hypoxemia. Despite supplemental oxygen, her SpO2 remains below the target range. NIV can provide higher levels of positive airway pressure and improve oxygenation without the need for invasive mechanical ventilation.
Avoidance of Invasive Intubation: NIV is a non-invasive intervention that can help prevent the need for endotracheal intubation and mechanical ventilation, which carries its own set of risks and complications. NIV allows for ventilatory support while maintaining the patient's airway and preserving their ability to communicate and protect their airway.
Patient Comfort and Compliance: NIV, delivered through a mask or nasal interface, is generally better tolerated by patients compared to invasive intubation. This is particularly important for patients like Maxine, who may feel anxious or uncomfortable with invasive procedures.
Customizable Settings: NIV can be adjusted to meet the patient's specific needs. In Maxine's case, the initial settings with an inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP) tailored to her condition aim to reduce her work of breathing and improve oxygenation.
Monitoring and Titration: NIV allows for continuous monitoring of the patient's response to treatment. If Maxine's condition improves or deteriorates, NIV settings can be adjusted accordingly. This real-time adaptability is essential in managing acute respiratory failure.
Patient-Centred Care: Maxine’s cultural and social background, being an Australian First Nations female, may influence her preferences and comfort with treatment modalities. NIV is generally more patient-centred and allows for communication and cultural considerations to be addressed.
High Flow Nasal Prong therapy could also be considered as an alternative therapy for Maxine if NIV is not available or not tolerated.
Further learning
- If you’re interested to learn how NIV would be initiated including selection of patient interface and initial settings, join us for the Lunch and Learn NIV webinar.
- Optimise your skills with Medcast's comprehensive course: PREPARED - Recognising and Responding to Clinical Deterioration
References
Rochwerg B, Brochard L, Elliott MW, et al. (2017). Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. European Respiratory Journal, 50(2), 1602426.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). (2021). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Retrieved from https://goldcopd.org/gold-reports/

Susan is the Head of Nursing Education for the Medcast Group.
DipAppScNsg, BN, CritCareCert, CoronaryCareCert, TraumaNsgCareCert, CertIV(TAE), MN(Ed), and GradCert(Ldrshp & Mgt).
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreMarjory is a 68 year old in-patient who is 2 days post hip replacement. She is on rivaroxaban (xarelto) for VTE prophylaxis. You find her sitting on the floor of the bathroom, alert but in pain.
We explore the case of Edward, a patient with acute kidney injury (AKI), focusing on renal protection strategies. It explores fluid management, blood pressure control, nephrotoxic drug adjustments, and electrolyte monitoring. Treatment considerations include vasoactive medications, dialysis options like CRRT, and medication dosing to support renal recovery and prevent complications.
James, a university student with a history of seasonal allergic rhinitis, presents with sudden respiratory distress following exposure to grass pollen during a soccer game shortly before a summer thunderstorm. Could this be thunderstorm asthma?
