Embracing Surgical Conscience: Essential ethics in perioperative nursing
As healthcare professionals, we navigate through complex surgical procedures, with each step guided by an unwavering commitment to patient care, safety, and integrity.
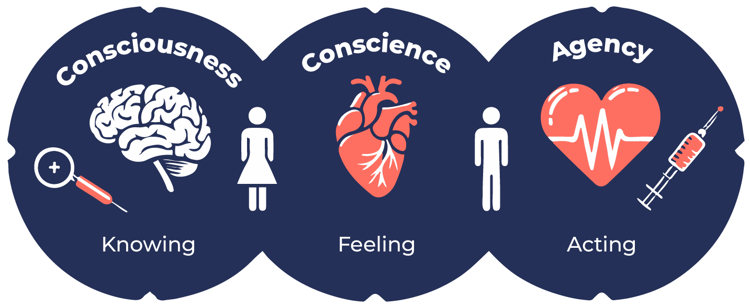
Surgical conscience refers to the ethical and professional responsibility of healthcare professionals to uphold the highest standards of patient care. It involves a strong commitment to adhere to established guidelines, protocols, and best practices while demonstrating a high level of personal accountability and self-awareness in the operating theatre.
Surgical conscience is more than just a buzzword - it is the ethical heartbeat that guides every cut, suture, and decision made by the surgical team. As patients entrust their lives to us, we are obligated to respect that trust and adhere to the four key principles that form the core of surgical conscience:

Adherence to surgical best practices
In Australian healthcare, the multidisciplinary team (MDT) is dedicated to following evidence-based guidelines and established surgical procedures. This commitment ensures the highest quality of care for patients, minimising the risk of adverse events. Adherence to guidelines includes thorough preoperative planning, precise surgical techniques, and vigilant intraoperative and postoperative care.
Patient autonomy and dignity
Beyond the physical act of surgery, the surgical team is responsible for respecting patient autonomy and preserving their dignity. This involves recognising patients' rights and involving them in decision-making processes. Upholding patient dignity is central to perioperative nursing in Australia, enhancing patient trust and comfort.
Transparency and honest communication
Honest communication is essential in perioperative care. It involves surgeons discussing the surgical procedure, risks, benefits, and expected outcomes with patients and their families. Perioperative nurses act as patient advocates, ensuring transparency and honesty throughout the surgical journey.
Continuous learning and improvement
Australians in the field of perioperative nursing are committed to ongoing education and staying abreast of advancements in surgical techniques, technologies, and relevant guidelines. This continuous improvement is crucial for delivering top-notch patient care.
“If mistakes happen during surgery, prompt reporting, open disclosure, taking responsibility and working to rectify the situation in the best interest of the patient must occur”
What is the impact of surgical conscience?
The influence of surgical conscience extends beyond the operating theatre. It fosters a culture of trust, leading to positive patient experiences and outcomes. In Australian healthcare institutions, it cultivates a collaborative environment, encouraging open communication, reducing medical errors, and inspiring ethical practice.
As we step into the operating room, let's remember that behind every mask lies a professional driven by the principles of surgical conscience. This commitment not only enhances our practice but elevates the standard of care for patients globally. In Australian perioperative nursing, surgical conscience is not just a concept; it's the ethical heartbeat of our profession.
Related courses and further learning
- Perioperative professional practice and the patient jouney: Perioperative Nursing Update Module 1
- Perioperative patient monitoring: Perioperative Nursing Update Module 2
- Perioperative therapeutics, from anaesthesia to analgesia: Perioperative Nursing Update Module 3
- Perioperative emergencies: Perioperative Nursing Update Course Module 4
- PACU protocols & Discharge Criteria: Perioperative Nursing Update Course - Module 5
References
Duff J., Bowen L., & Gumuskaya O., (2022) What does surgical conscience mean to perioperative nurses: An interpretive description. Collegian Vol 29 (2) https://doi.org/10.1016/j.colegn.2021.07.007
Quintana D. (2022) Surgical Conscience: A concept analysis for perioperative nurses. AORN Journal Vol 116 (6) https://doi.org/10.1002/aorn.13827
Quintana D. (2023) The Importance of Having a Surgical Conscience AORN https://www.aorn.org/article/the-importance-of-having-a-surgical-conscience December

DebEvans, RN, BSc, DipAnaes&PostAnaesNsg, CritCareCert, DipProfStudies, Teach&AssessClin.PractCert, CertIV(TAE) has extensive background in Perioperative education and management. Deb has worked overseas and in several tertiary hospitals in Brisbane as an educator and manager including the Mater & The Wesley Hospital where she was awarded CEO Award for Innovation and Excellence and The Spirit of Wesley Staff Award for commitment to Quality and Safety.
Deb has developed blended education programs within the perioperative environment to include; Graduate transition programs; Clinical mandatory training; Corporate required learning & Point of Care SIMs; Perioperative competency development skills and speciality training programs. She recently worked for Montserrat Day Hospitals as the National Education & Training Manager and implemented a virtual orientation program, LMS & introduced speciality learning pathways. Deb has also been an ALS instructor & involved with a range of universities as a clinical facilitator and a lecturer at TAFE.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreSeeking guidance on which courses to prioritise before the CPD year concludes? You're not alone! Essential CPD for Australian nurses covering skills, patient care & standards.
Once anaphylaxis has been identified, immediate treatment is required to stop the allergic cascade from producing histamines, prostaglandins and cytokines, and manage the effects of these agents. Management will include immediate treatment, refractory management and post crisis management.
Billy is 8 weeks old, he was born NVD and is up to date with his immunisations. He has been vomiting for the last 3 weeks and is very irritable with a high pitched cry.
